If you are suffering from back pain or leg pain caused by your spine, you may wonder if there is a difference between bulging disc vs. herniated disc. These two terms are often used interchangeably because they are fundamentally the same thing: damage to a disc that presses on a nerve and causes pain in the back and/or the legs (or arms, if the damaged disc is in the neck).
While these two conditions are similar, they are not technically the same — although that probably doesn’t matter to you if you are experiencing pain from either of these conditions! Let me explain more about bulging disc vs. herniated disc and the best treatment options for both.
What’s the difference between bulging disc vs. herniated disc?
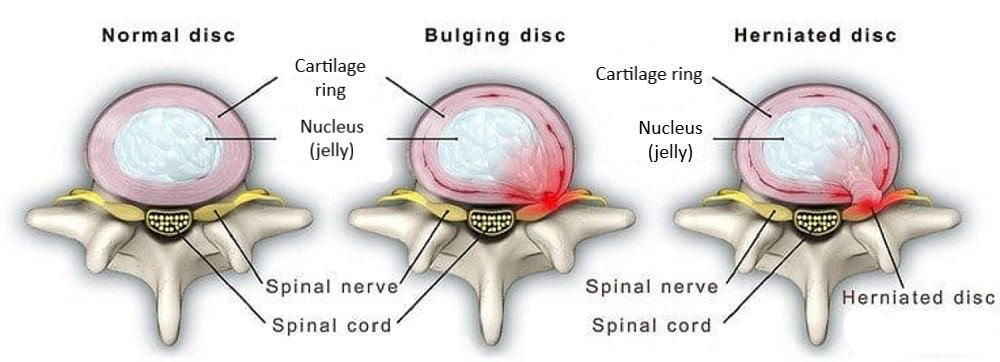
The main difference between bulging disc vs. herniated disc is the extent of damage to the disc. Think of your discs as jelly donuts that lie next to your vertebrae, with your spinal nerves running between the two. A bulging disc results when the jelly-like inner layer of the disc pushes against the outer layer of the disc, which then pushes on the nerve and can cause pain. A herniated disc occurs when the outer layer of the disc tears or cracks and the inner layer leaks out and pushes on the disc, also potentially causing pain.
Both bulging discs and herniated discs are types of degenerative disc disease. Disc degeneration is caused by injury, aging, regular physical labor, or sitting or standing for extended periods. Growing older is the most common cause of bulging and herniated discs. In fact, everyone over the age of 40 has some form of degenerative disc disease, according to the Arthritis Foundation.
While most adults will experience disc degeneration, not everyone will experience pain. If a bulging disc or a herniated disc causes symptoms, most people will experience pain radiating in the back and/or down the leg or arm (depending on where the disc problem occurs). The pain can be steady, or it could increase when sitting and decrease when walking. Some people also may experience muscle weakness, spasms, or tightness. In my experience, a herniated disc is more likely to cause pain because there is an actual tear in the outer layer of the disc.
Bulging disc vs. herniated disc are commonly used interchangeably as they are very similar. Only imaging can distinguish between a bulging disc and herniated disc. MRI, CT scans, and X-rays can be effective in identifying bulging discs and herniated discs.
What are treatments for bulging disc vs. herniated disc?
Most of the time, bulging disc and herniated disc follow the same course of treatment. At Neurosurgery One, we almost always begin with conservative treatment, such as steroid injections, unless you are experiencing any red flag symptoms that require immediate intervention. In fact, our spine team includes interventional pain management physicians who specialize in non-surgical treatments for spine pain, so you don’t even have to leave our practice to get the care that’s best for you.
If surgery is necessary, bulging disc surgery is most often a minor surgical invention. A microdiscectomy or endoscopic discectomy are the most common surgeries for bulging discs. These minimally invasive spine surgeries remove the protruding part of the disc that is compressing the nerve.
A patient with a herniated disc also can be treated with a microdiscectomy, but they may need more invasive surgical intervention, particularly if the herniated disc is causing loss of bowel or bladder function or pain into the leg. Like a microdiscectomy or endoscopic discectomy, a traditional discectomy removes the damaged part of the disc; however, it is performed through a larger incision.
In a study of patients who underwent a microdiscectomy, endoscopic discectomy, or a laminectomy/laminotomy with discectomy for their lumbar disc herniation, 79% had good or excellent results. For patients who underwent an anterior cervical discectomy and fusion (ACDF) for disc herniation in the neck, or cervical area of their spine, upwards of 95% self-reported success.
What are the differences between slipped disc vs. herniated disc?
In addition to bulging disc vs. herniated disc, you also might wonder about slipped disc vs. herniated disc. These are actually one and the same. Slipped disc is a more casual term for herniated or ruptured disc. Slipped disc may be used more frequently for patients with spondylolisthesis, which is when a vertebra (the bone portion of your spine) slips forward over the vertebra below it.
The treatment for slipped disc is the same as it is for a bulging disc or herniated disc. Ice, rest, and pain medications are usually the first line of treatment, and some patients may progress to physical therapy if necessary. Upwards of 90% of patients with slipped disc or herniated disc do not need surgery, according to a research analysis.
When should I seek treatment for bulging disc vs. herniated disc?
The vast majority of patients benefit from conservative treatments. If you believe you have a slipped, herniated, or bulging disc and have symptoms that are interfering with your daily life, you should first see your primary care provider. In most cases, ice, rest, pain medications, and physical therapy will likely help alleviate your pain and symptoms. If your condition does not improve in 6-8 weeks, your doctor will most likely refer you to a neurosurgeon for a spine consultation where we can discuss next steps such as spinal injections vs. surgery.
If you have loss of bladder or bowel function, leg or arm weakness, or severe pain, you should seek medical care immediately. This can indicate severe damage to your spine or nerve, and your condition must be treated immediately to avoid long-term damage.



