If you have chronic low back pain, what can you do when physical therapy and medications don’t work? For years, patients have been diagnosed non-specific low back pain. It’s a dreaded diagnosis both for doctors to give and patients to hear because it basically means that there is no clear cause of your pain. And without a cause, there is no treatment.
But for some patients with chronic lower back pain, there actually are causes that have been overlooked that can now be treated with new minimally invasive procedures that avoid lumbar spinal fusion. The two causes that can now be treated are fairly easy to diagnose once you are looking for them. They are:
- Multifidus muscle dysfunction: This condition – often described by patients as a tight back – occurs when the muscles that support the lower back “shut off” in response to back strain and pain. This leads to spinal instability and further pain and strain as other muscles try to compensate.
- Vertebrogenic pain (also called vertebral endplate nerve dysfunction): This condition — which can occur simply as a result of normal aging — is when the layer of nerve-packed cartilage that separates the vertebra (bone in the spine) from the disc (padding between bones) becomes compressed and causes pain.
New minimally invasive therapies for chronic low back pain
The good news is that both of these conditions can be easily diagnosed through an MRI and both can be treated with new minimally invasive procedures. Multifidus muscle dysfynction can be treated with rehabilitative neurostimulation that reactivates the muscle. Vertebrogenic pain can be treated with a procedure called basivertebral nerve ablation that stops the affected nerve from transmitting pain signals. Both treatments are approved for patients with chronic low back pain that hasn’t responded to PT or medications, if an MRI shows the cause is either due to multifidus dysfunction or vertebrogenic pain.
Both procedures have similar benefits:
- performed as outpatient procedures, allowing you to go home from the hospital on the same day
- FDA-approved, with medical evidence supported in peer-reviewed studies
- help prevent the need for lumbar spinal fusion
Restoring lower back muscle function reduces pain
Low back pain that doesn’t respond to PT or medications could be mechanical in nature. When chronic low back pain is mechanical rather than nerve-related, it often involves a group of deep spinal muscles called the multifidus. Over time, the multifidus muscle can “shut off” in response to back strain and pain. This leads to spinal instability and further pain and strain as other muscles try to compensate, according to a study published in Neuromodulation journal. This condition can occur alongside diagnosed spinal conditions, such as degenerative disc disease, and persist even after spine surgery.
This process is called arthrogenic muscle inhibition (AMI). When there is pain in a joint, AMI can kick in, lowering the activity of the nerve cells that control the muscle that moves or stabilizes that joint.
In cases of ongoing low back pain, imagine AMI as a boss who tells the multifidus muscle to take a leave of absence. This leaves the spine with less structural support, forcing other muscles to compensate, which triggers more lower back tightness and pain.
While the multifidus is on leave, it kicks back and becomes weaker and starts to atrophy. Often, no amount of coaxing through physical therapy can make it start working again.
 A new procedure called ReActiv8 can help solve this problem. ReActiv8 is an implantable neurostimulator, kind of like a pacemaker, that forces the multifidus to go back to work. When the low back muscle starts working again, it helps strengthen and stabilize the spine, which reduces the pain.
A new procedure called ReActiv8 can help solve this problem. ReActiv8 is an implantable neurostimulator, kind of like a pacemaker, that forces the multifidus to go back to work. When the low back muscle starts working again, it helps strengthen and stabilize the spine, which reduces the pain.
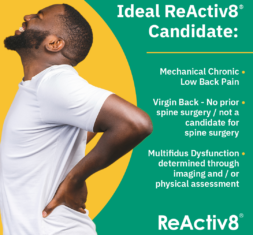
ReActiv8 is considered a restorative therapy; over time it restores the normal muscular recruitment and movement of the multifidus muscle. ReActiv8 is FDA-approved for use in patients with multifidus atrophy diagnosed through MRI or physical exam using a prone instability test and a multifidus lift test.
Think of it like internal PT for your low back muscles!
In clinical trials, people with ReActiv8 have seen progressive long-term improvements in pain and function. At the two-year mark, three out of four participants (76 percent) reported substantial improvements in pain, disability, or both, and 60 percent of patients on opioids had voluntarily reduced or eliminated their intake.
Turning off nerves sending pain signals from the lower back
A completely different cause of chronic low back pain is called vertebral endplate nerve dysfunction. This condition causes vertebrogenic pain, which is low back pain that originates from the bones of the spine (vertebrae) rather than the discs. Interestingly, many patients with this condition have been told that their pain is being caused by a disc when that’s not the case.
The vertebral endplate is a small layer of cartilage, packed with nerves, that separates the bone of the vertebrae and the disc. Vertebral endplate nerve dysfunction happens when the endplate and those nerves become compressed, causing a great deal of pain. This condition is often not found until a spine surgeon who specializes in this problem diagnoses it.
Even though vertebral endplate dysfunction has been under study for more than 30 years, many physicians remain unfamiliar with the diagnosis and its signs and symptoms. Often, radiologists don’t pick it up on MRIs, or the MRI is not extended far enough down the spine to spot the problem.
That’s how most patients with chronic low back pain end up with a misdiagnosis of degenerative disc disease or, worse, something called “non-specific” lower back pain. In fact, up to 85% of patients are diagnosed with “non-specific” lower back pain. That’s a problem, because if a patient isn’t getting the correct diagnosis, they’re also probably not getting the correct treatment.
On a spinal MRI, I look for a finding called Modic changes, in which the bone marrow becomes inflamed and swells, or the bone marrow turns to fatty tissue due to reduced blood flow. This indicates vertebral endplate nerve dysfunction, which can be effectively treated with a minimally invasive procedure called Intracept.
 During the Intracept procedure, I use radiofrequency energy to ablate, or destroy, the nerve that is transmitting pain signals to your brain. This nerve, called the basivertebral nerve, is unique because it does not regenerate like other nerves in the body. Because it cannot regrow and begin transmitting pain signals again, there should be no need to repeat the Intracept procedure. A majority of patients reported 75% to 100% pain reduction at five years after the Intracept procedure, according to Relievant Medsystems, the maker of Intracept.
During the Intracept procedure, I use radiofrequency energy to ablate, or destroy, the nerve that is transmitting pain signals to your brain. This nerve, called the basivertebral nerve, is unique because it does not regenerate like other nerves in the body. Because it cannot regrow and begin transmitting pain signals again, there should be no need to repeat the Intracept procedure. A majority of patients reported 75% to 100% pain reduction at five years after the Intracept procedure, according to Relievant Medsystems, the maker of Intracept.
There is very little risk to ablating the basivertebral nerve; it does not impair any function. However, in the unlikely event that you were to break that vertebra, you might not know it because you wouldn’t feel any pain. Because of this, I tell my patients that if they experience a fall, car crash or other type of accident, they should be sure to get the scan that is normally recommended to check for fractures.
Re-assessing your chronic lower back pain
I love offering new technology to patients if it is safe, has a good scientific basis, and has good outcomes. Intracept and ReActiv8 check all three of those boxes. And they are bringing welcome relief to patients who thought they had no other option than to live with their pain.
I recommend getting a fresh assessment of the cause of your pain if you have:
- Experienced low back pain for six months or longer
- Tried physical therapy, medications or other conservative treatments without adequate pain relief
If you have had an MRI done, you don’t even need to come in person for an evaluation. You can submit your imaging and schedule a telehealth consultation to review your health history and discuss whether your pain is being caused by a condition that could be treated with one of these new procedures. Of course, if you haven’t had an MRI or you would like to see me in person, I’m happy to schedule an appointment in either our Lone Tree-Yosemite or Castle Rock offices.
Request an appointment online or call our main number: 720-638-7500, Option 4, and let my scheduler know which type of appointment you would prefer. I typically can see new patients within a week.
If you are a candidate for either ReActiv8 or Intracept, the medical companies that developed the technology have authorization teams that will help get insurance approval for the procedure.



