Chronic low back pain is frequently diagnosed as a disc problem, but the real culprit may be in the bones of your spine. Many patients with chronic lower back pain are diagnosed with degenerative disc disease, a term used to describe wear and tear on the padding between the vertebrae. Patients diagnosed with this condition typically are treated with some combination of over-the-counter medication, opioid painkillers, physical therapy, spinal injections, and even surgery. And yet, they still don’t find long-term relief for their low back pain, because many of these patients have been misdiagnosed.
Rather than stemming from the disc, chronic low back pain frequently stems from the vertebrae itself. Pain that originates at the disc is called discogenic, whereas pain coming from the bone is referred to as vertebrogenic back pain. But the type of vertebrogenic back pain responsible for most cases of chronic back pain is only starting to be recognized.
It’s called vertebral endplate nerve dysfunction, and while it’s been under study for more than 30 years, many physicians remain unfamiliar with the diagnosis and its signs and symptoms. That’s how most patients with chronic low back pain end up with a misdiagnosis of degenerative disc disease or, worse, something called “non-specific” lower back pain. In fact, up to 85% of patients are diagnosed with “non-specific” lower back pain. That’s a problem, because if a patient isn’t getting the correct diagnosis, they’re also probably not getting the correct treatment.
The Real Cause of Chronic Low Back Pain
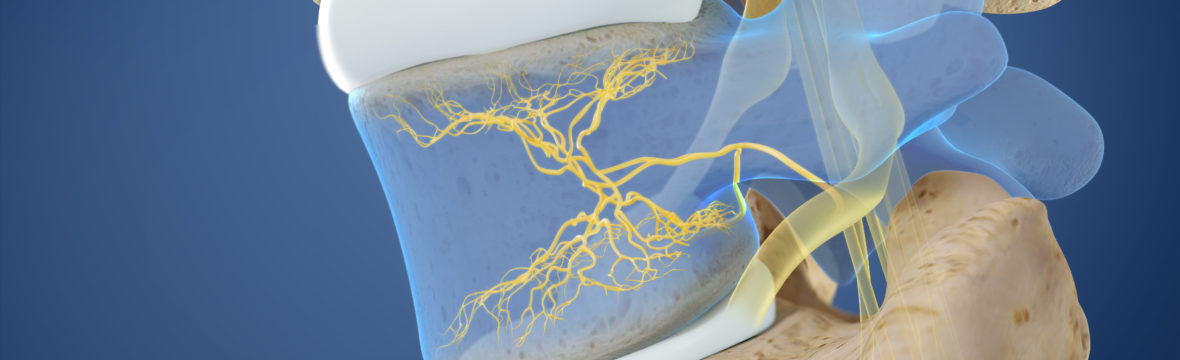
Separating each vertebrae and spinal disc is a thin layer of cartilage called the vertebral endplate. It’s small—between 0.1 and 2 millimeters thick—yet it’s packed with nerves. Vertebral endplates are much more nerve-dense than spinal discs, which means they’re more susceptible to pain than discs. Vertebral endplate nerve dysfunction is when the endplate and the nerves within it become compressed, causing a great deal of pain. The compression is a natural side effect of years of wear and tear, and becomes more common as we age.
Vertebral endplate nerve dysfunction is often mistaken for degenerative disc disease because of the proximity of the disc to the endplate. If a radiologist isn’t trained in vertebral endplate nerve dysfunction, it’s easy to miss the signs on imaging.
Diagnosing Vertebrogenic Back Pain
A patient’s true cause of chronic back pain can be determined using MRI. If the pain is because of vertebral endplate nerve dysfunction, the MRI will show what’s called Modic changes. There are two types of Modic changes that indicate vertebral endplate nerve dysfunction:
Type 1: Bone marrow becomes inflamed and swells.
Type 2: Bone marrow turns to fatty tissue due to reduced blood flow.
If a patient has chronic low back pain lasting 12 weeks or longer and has type 1 or type 2 Modic changes, he or she has vertebral endplate nerve dysfunction. But because many radiologists still aren’t looking for Modic changes on MRI, patients with chronic low back pain need to advocate for their own care to get a proper diagnosis. If low back pain persists for six months or longer and doesn’t respond to treatment, patients should get a second opinion from a physician specially trained in vertebral endplate nerve dysfunction.
Good News About Vertebrogenic Back Pain
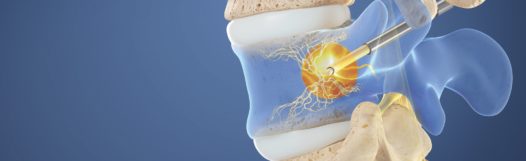
The good news for patients with vertebral endplate nerve dysfunction is that the condition can be treated with the new Intracept basivertebral nerve ablation procedure. Basivertebral nerve ablation is a minimally invasive treatment during which a spine doctor uses radiofrequency energy to destroy the nerve in the vertebral endplate that is transmitting pain signals to the brain.
The Intracept procedure is quick. I generally have patients heading home within three hours of arrival, and that includes recovery time. And it requires very little downtime afterwards. I recommend patients take it easy the rest of the day of the procedure, but then most patients can return to work and their regular routines the following day. The best part is, it’s long-lasting. Because the basivertebral nerve does not regenerate like other nerves in the body, patients don’t need to worry about it growing back. And that means there’s no need for repeat procedures. In fact, most patients’ pain continues to improve over time with the majority reporting 75% to 100% pain reduction five years after the procedure.
Who Should Be Assessed
If you suffer from lower back pain, you should be assessed to detect whether the cause could be vetebrogenic in nature if you answer “yes” to these three questions:
- Have you had lower back pain for six months or longer?
- Have you tried conservative treatment, such as physical therapy or medication, for at least six months and it has not helped?
- Have you been told your lower back pain is caused by “non-specific” or discogenic issues?
You also should be assessed for vertebrogenic lower back pain if you are just seeking medical care and have not yet had a diagnosis. Currently, we see patients for this condition in our Lone Tree and Castle Rock medical offices and usually can schedule an assessment within 10 days.
Intracept Procedure Video