Drug-Resistant Epilepsy Patients Face 20-Year Delay in Surgery Referral

By Dr. Abhijeet Gummadavelli: Adult Epilepsy Specialist, MD
Abhijeet Gummadavelli, MD, is a fellowship-trained neurosurgeon with Neurosurgery One in Littleton. He specializes in stereotactic and functional neurosurgery as well as spinal cord stimulation and a variety of spinal and brain surgeries. He has nearly a decade of neurosurgery experience and recently completed a fellowship in stereotactic functional and epilepsy neurosurgery at Vanderbilt University Medical Center.
Key Take-Aways:
-
40% of patients suffer from medically refractory epilepsy
-
There is over a 20-year delay in surgical referral
-
Patients should be referred for surgical evaluation without delay after failing 2 anti-seizure medications, as evidence shows additional medications have higher failure rates
-
Patients with longer epilepsy duration prior to intervention do not see equal improvements in quality of life and mood as those with earlier intervention
An estimated 1.2 million American adults have epilepsy that is uncontrolled by anti-seizure medications. That equates to 4 out of every 10 adults with epilepsy. While surgery is potentially life-saving for any of them, most will not be evaluated for surgery on average for more than 20 years after becoming eligible.
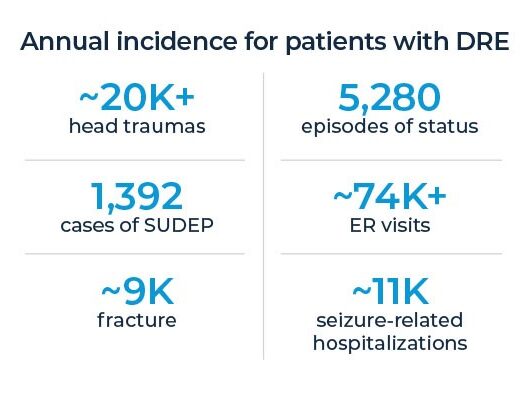
This delay in surgical evaluation results in:
- increased risk of head trauma, ER visits and hospitalizations
- increased risk of SUDEP
- increased depression, anxiety and sleep disturbance
- cognitive and memory impairment
- lower earnings
- reduced benefit after surgical intervention
Patient Referral Criteria
The criteria for patients to be candidates for surgical evaluation are very simple:
- They must have uncontrolled epilepsy, which is defined as 1 seizure within a one-year period.
- They must have had 1 seizure after trying two appropriately dosed and tolerated anti-seizure medications.
These criteria are where the biggest delays in referrals occur whether due to patient or referring provider misperceptions.
Myth 1: Many patients compare themselves to some imaginary standard, saying to themselves, their families and their providers that their epilepsy is “not that bad” or “is tolerable.” (Some may not even report seizures in the false belief that nothing more can be done.) However, both empirical and anecdotal evidence shows that this is not the case and that is why the definition of uncontrolled epilepsy is just a single seizure in a one-year period.
Myth 2: The second misperception is the belief that a different anti-seizure medication using a different mechanism might be the answer. With more than 30 medications available, on the surface, this seems to make sense. However, again, the evidence doesn’t bear this out. In fact, the evidence has repeatedly found that the likelihood of seizure freedom decreases dramatically after two anti-seizure medication trials, resulting in the International League Against Epilepsy’s definition of treatment resistance as “failure of adequate trials of two tolerated, appropriately chose and used antiepileptic drug schedules to achieve sustained seizure freedom.”
Benefits of Early Referral of Medically Refractory Epilepsy Patients
Patients who meet these two criteria should be referred as soon after the second drug failure as possible to a comprehensive epilepsy program that includes an epileptologist, epilepsy nurse navigator, neuropsychologist, neuroradiologist, and neurosurgeon along with an epilepsy monitoring unit. These patients will receive in-depth, advanced testing and be presented at epilepsy conference to consider the best pathway of care, including nonsurgical and surgical options.
For the 1.2 million drug-refractory epilepsy patients, surgery can be life-saving. But even for the few who do not qualify for surgery, surgical evaluation can enhance the care through improvement in diagnosis, optimization of therapy, and treatment of comorbidities.
Expedited Referrals for Your Medically Refractory Epilepsy Patients
Once a patient has failed two appropriately dosed and tolerated anti-seizure medications, referral to an epileptologist or comprehensive epilepsy program can be difficult due to the wait times in the Rocky Mountain region. To help accommodate referrals and faster evaluation, Neurosurgery One and AdventHealth Littleton are working together to expedite this process.
Due to our comprehensive program, referring providers can refer patients to Neurosurgery One or the Epilepsy Program at AdventHealth to obtain a multi-disciplinary evaluation by an epilepsy team that includes an epileptologist, epilepsy nurse navigator, neuropsychologist, neuroradiologist, and neurosurgeon. At epilepsy conference, this team reviews individual patient cases and quickly directs the patient into the right pathway of care.
To make a referral to Dr. Abhijeet Gummadavelli at Neurosurgery One, please use one of these options:
- Refer online using this HIPAA-compliant form
- Call our epilepsy evaluation schedulers directly:
- Lauren Ortega: 720-638-7517
- Chanel Love Leewaye: 720-922-6483
Or make a referral to the Epilepsy Program at AdventHealth Littleton using this form.